Diagnosing Medicaid Drug Overspend in the Commonwealth Part I
An Analysis of Virginia Medicaid Prescription Drug Spending 2017-2023
Introduction
In the Commonwealth of Virginia, the Department of Medical Assistance Services (DMAS) contracts with Managed Care Organizations (MCOs) to manage the healthcare benefits of Medicaid enrollees. These MCOs then contract with Pharmacy Benefit Managers (PBMs) for the administration of medication related benefits by negotiating manufacturer rebates, enforcing the state formulary, and processing drug claims. Many MCOs and PBMs are vertically integrated, meaning they are part of a larger company that own health plans, pharmacies, and health systems.
With the increasing cost of medication for the Virginia Medicaid program and the growing number of pharmacy deserts in Virginia, it is imperative to find solutions that address medication cost and pharmacy access immediately. To identify these solutions, an in-depth analysis was performed using drug payment and pricing data reported to the Centers for Medicare and Medicaid Services (CMS).
To seek solutions to this problem, an analysis was conducted using the Medicaid and CHIP Payment and Access Commission (MACPAC) Databooks, National Drug Acquisition Cost (NADAC), and the CMS State Drug Utilization Data (SDUD) submitted by Medicaid programs each quarter. These sources are critical not only for the accuracy and accountability they provide, but also because these reports come from datasets that are used to inform policy, calculate drug reimbursement, set managed care capitation rates, and determine manufacturer drug rebates.
Findings
Medical Total Spending
Virginia Medicaid spent $2.21B more than they should have in 2023 when compared to the national medicaid average per enrollee.
Net Drug Spending
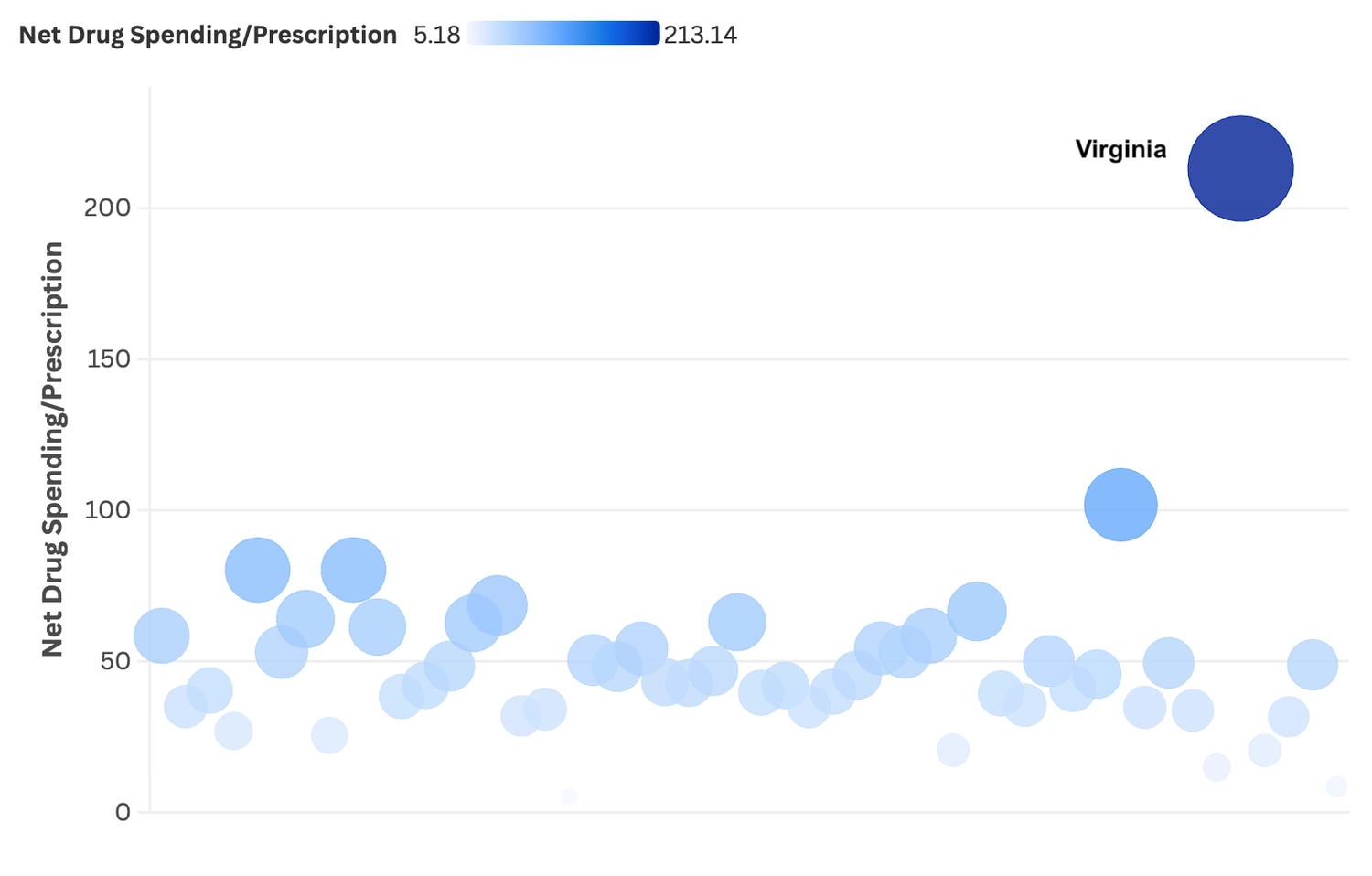
The entire amount of this overspend can be attributed to prescription medications. If the Commonwealth would have paid the national average net cost (gross cost minus manufacturer drug rebates) per prescription, it would have saved $3.65B in 2023 and $10.86B since 2017.
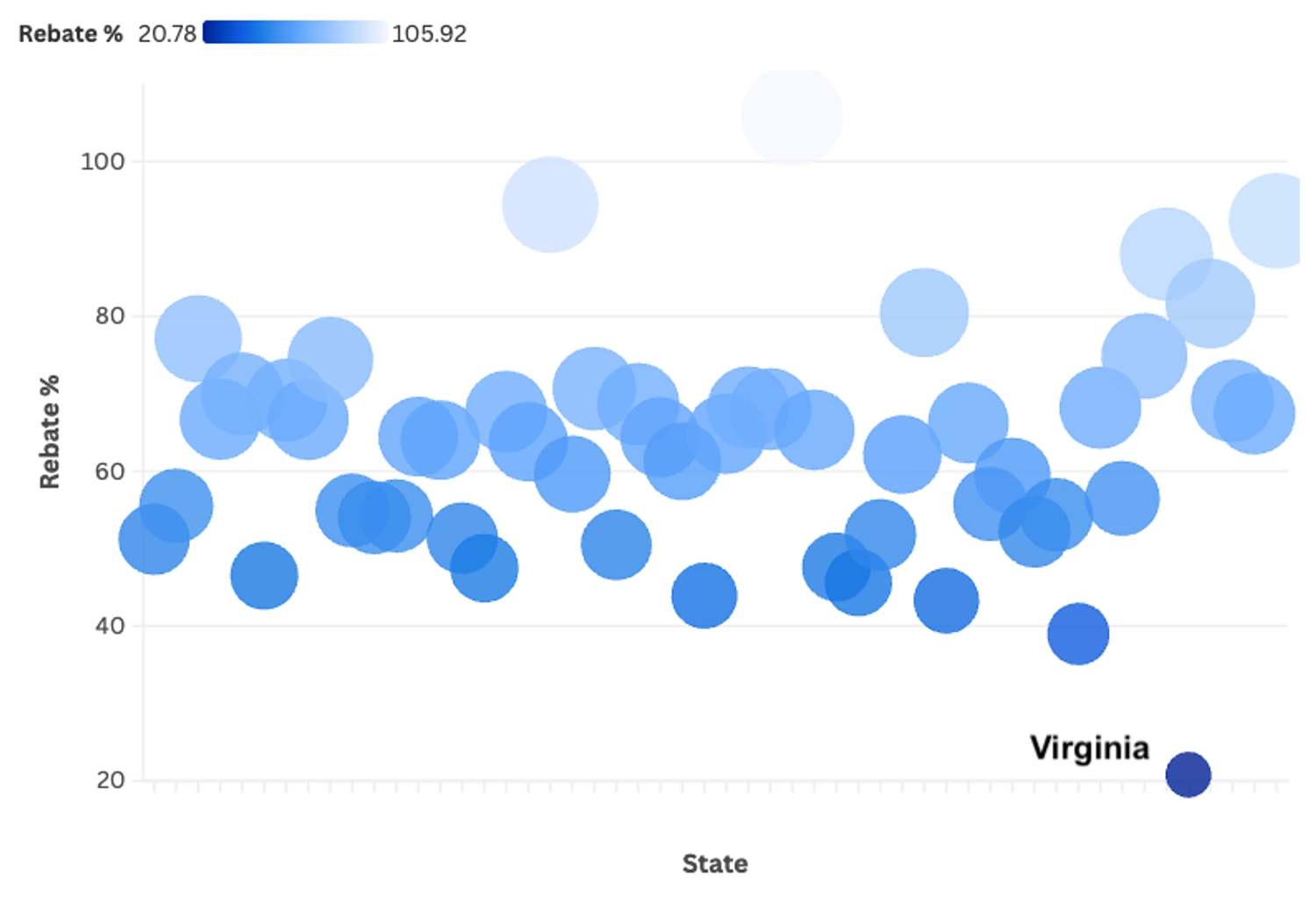
Drug Rebates
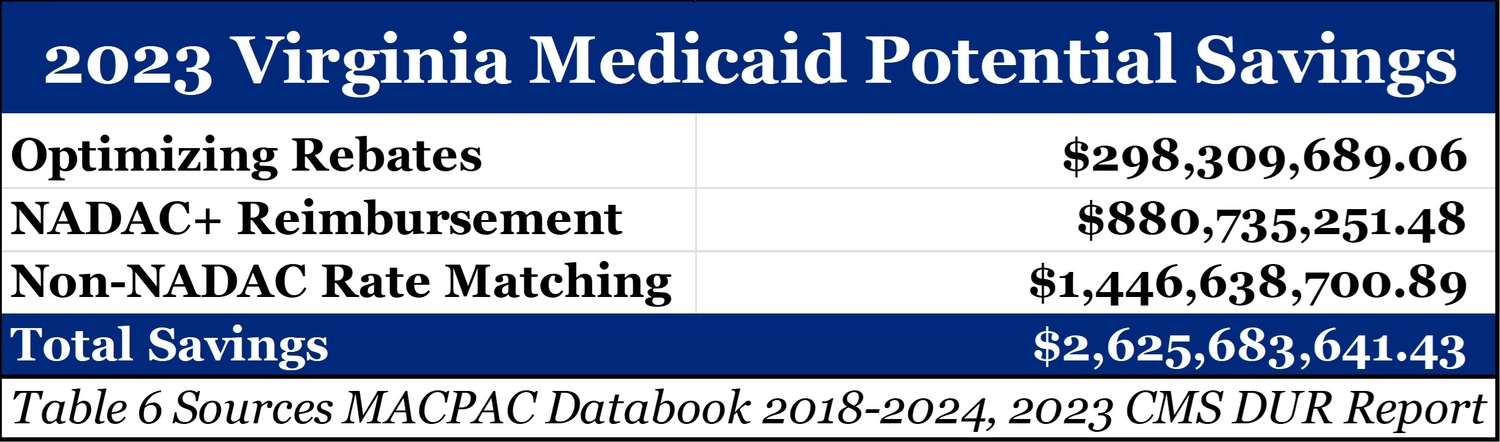
Drug rebates being retained by intermediaries such as Group Purchasing Organizations (GPOs), MCOs, and PBMs, are only a fraction of the problem. While Virginia is last in the country with only 20% of gross drug spending being returned in the form of a manufacturer rebate, the data suggests only $298.3MM would have been saved by optimizing rebates in 2023. The overspend is an issue of over payment rather than a lack of discounts.
Brand VS Generic Spending
This is made further evident when examining brand versus generic spending. Matching the national average for net brand drug spending per prescription would have only accounted for $449.9MM in overspend in 2023.
Generic drug spending has increased from $33 per prescription in 2018 to $156.40 in 2023. Considering the national average is only $23.31 prescription, Virginia Medicaid spent $2.82B more on generic drugs in 2023 than it should have and $8.23B since 2017.
NADAC + Analysis
This level of spending can be addressed immediately via executive order for all medicaid plans to set reimbursing for drugs with a National Drug Acquisition Cost (NADAC) number to NADAC plus the state cost of dispense determined by survey (NADAC+). In 2023, the NADAC+ model would have saved Virginia Medicaid $880.7MM. 98.5% of these savings come from generic drugs.
Non-NADAC Drugs
There were $3.73B in 2023 Virginia medicaid claims for drugs without a NADAC number. To analyze these drugs, we compared how much Virginia MCOs paid for each individual drug identifier (NDC) per unit and matched it against the Virginia fee-for-service (FFS) program and North Carolina MCOs.
While there were only $1.2B worth of NDC matches with the Virginia FFS program, if MCOs had paid at the FFS rate it would have saved the Medicaid Program $790.6MM in 2023.
When comparing MCO spending on non-NADAC NDCs to North Carolina Medicaid MCOs, there were $2.57B worth of NDC matches. If these NDCs were paid at North Carolina MCOs rates, it would have saved Virginia Medicaid $1.39B in 2023.
When combining all three datasets, there exists a potential overspend of $1.45B by Virginia Medicaid MCO plans for non-NADAC medications.
Conclusions
In no Medicaid program is overspending on medication more apparent than in Virginia Medicaid. Medicaid plans have over-spent by $10.86B on medication vs. the national average on a per prescription basis in the years 2017 through 2023. This overspend is almost entirely due to overpayment for generic medications in Medicaid MCO plans with 98% of the overspend happening after the start of 2019.
Notably, 2019 is the year that spread pricing, the act of PBMs retaining payments meant for pharmacies, was abandoned by 4 of the 6 MCOs in in the Commonwealth Medicaid program. 2019 and 2020 Also saw large market consolidation and vertical integration in Virginia Medicaid MCO plans with net cost of medication per prescription having quadrupled in the two years since 2018. In 2023, the net cost had risen 617% from 2018 levels to $213.14. During the same timeframe, MCO spending on generic drugs increased 452% per prescription from $34.82 to $157.44.
In Part II of this report, we will explore the mechanisms allowing for this overspend, characteristics of the high margin medications responsible, and where this money is and is not going.
Recommendations
To bridge the gap between what Virginia Medicaid is spending per enrollee and the national average, prescription drug reimbursement must be addressed. The data indicates prescription drug spending under MCO plans account for the $2.21B in 2023 in total Medicaid overspend. Through rebate optimization, NADAC+ reimbursement, and rate matching on non-NADAC drugs, the Commonwealth has an opportunity to be better than the national average by creating savings of $2.63B.
Single PBM Implementation
Rebates and non-NADAC drug spending can be addressed by the continuation of work on DMAS utilizing a single PBM. Contracting with a single transparent PBM will give Virginia Medicaid the ability to ensure savings are being maximized and resources are allocated appropriately.
NADAC+ Reimbursment
Immediate savings can be realized by executive order for DMAS to give MCOs a 30-day notice to change reimbursement to a NADAC+ model for all NADAC drugs. The state would save an estimated $881MM per year and address the growing number of pharmacy deserts.
Claims Transparency
The Commonwealth should also make claims information more transparent by allowing greater access to claims information. As it stands now, the law prevents everyone, lawmakers and government officials included, from accessing claims details.
Thank You
Thank you to everyone whose time and insight helped make this report happen. Pharmacists United for Truth and Transparency, Cindy Warriner, Antonio Ciaccia, Mike Sharp, Greg Reybold and Otto Wachsmann just to name a few. The insight and direction you all gave me was invaluable. Thank you as well to PharmacyHub for this report page and interactive graphs, PUTT and GRX marketing for the PDF designs, my mother, father, and the friends that I cannot name.
And a special thanks to my wife Emily and daughter Ellison, who have been patient with me for the months it took to make sure this was done right. I love you both and doing all I can do to do the right thing.
Jeremy Counts, PharmD
Chief Analyst
